Health Literacy: Improving Outcomes by Keeping Patients Informed

A common and unfortunate situation that many patients find themselves in is having a physician explain something only for the patient to not understand what was said.
Picture it: a patient’s sitting in their doctor’s office after recently having surgery. The doctor begins explaining the appropriate aftercare instructions to the patient, however, the instructions are full of jargon, unclear, or don’t quite make sense.
The doctor may assume that the patient understands everything, or they might get called away before the patient can ask any questions. Or, just as likely, the patient nods along with the instructions, because they don’t want to burden the doctor by making them repeat themselves or further explain the instructions.
What can a doctor do to avoid these situations, and ensure that the patient fully understands the scope of their treatment?
What is Health Literacy?
Health literacy is an individual’s ability to access, process, and understand basic information about their health. There are many factors that contribute to an individual’s health literacy, including the person’s general literacy levels – the ability to read, write, and understand written information.
Other factors include (but are not limited to):
- Experience levels with healthcare systems
- The type of communication
- The communication method
- The culture of the person and of the healthcare organization relaying the information
For patients and providers, improved health literacy would mean improved levels of disease management, as well as reduced provider utilization due to lower patient admittance and readmittance rates.
In recent years, medicare enrollees with “adequate” health literacy saw 4% fewer hospitalizations over a three-year period than those with “basic” or “below” basic health literacy levels. To add to this, it was observed that 33% of patients with “adequate” health literacy had a stable control of their diabetes versus 20% for patients with “basic” or “below” basic levels of literacy.
What are the Implications of Limited Health Literacy?
The National Center for Education Statistics performs a National Assessment of Adult Literacy (NAAL) every 10 years.
This survey shows four levels of literacy:
- Proficient
- Intermediate
- Basic
- Below Basic
Although more than half of the adult patients in these surveys regularly show adequate levels of health literacy, many patents struggle to understand healthcare.
The following are a few points from the most recent (at the time of writing) NAAL survey:
- 26% of participants didn’t know when their next appointment was scheduled for
- 42% of participants didn’t understand their prescription’s instructions
- 78% of participants misinterpreted the warning labels of their prescriptions
How to Tell if a Patient has Limited Health Literacy
Based on the above mentioned NAAL study, there are approximately 89 million American adults that have limited health literacy.
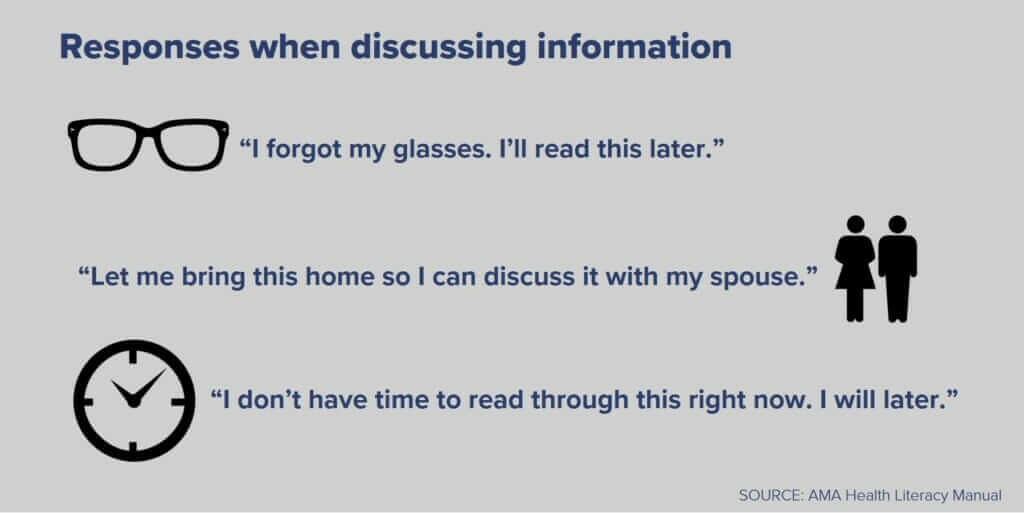
Every day, physicians see patients who have trouble reading and understanding health information. Some clues that patients might be struggling are:
- Constantly missed appointments
- Lack of follow through with laboratory and/or imaging tests
- Lack of response to referrals
- Non-compliance with medication regimens
Providers should also gather demographic data, as this can indicate risk among patients who are elderly, unemployed, lack a high school diploma or education, have no insurance, don’t speak English, speak English as a second language, or have low (or no) income, as these patients may be at an increased risk of experiencing low health literacy rates.
How Providers Should Handle Patients with Low Health Literacy
Regardless of whether a provider is working with a patient face-to-face or providing care remotely, they should be asking all patients if they need help reading or understanding their instructions or other written materials.
Providers should also actively work on enhancing both their verbal and written communication.
6 Steps for Enhancing Verbal Communication with Patients
Verbal communication has been observed to decrease the rates of stress, anxiety, and pain that patients experience. It can also help to improve patient satisfaction and increase compliance.
The following are 6 steps that providers can use to help improve verbal communication with patients:
- Slow down and speak calmly
- Avoid jargon and use plain, simple language
- Use visuals when necessary and available
- Explain (and repeat) the most important concepts
- Teach-back; encourage the patient to reiterate the information
- Encourage questions constantly
5 Guidelines for Enhancing Written Communication with patients
While verbal communication helps patients feel more comfortable, physicians often need to write content or instructions down for future reference.
When doing so, it’s important to use patient-friendly language. When interacting with patients remotely, providers need to make sure that they’re using technology that allows them to speak with the patient in a plain language.
When writing instructions or any other content for a patient, it’s important to follow the following 5 guidelines:
- Write at or below a sixth grade reading level
- Use one or two syllable words when possible, and stick to an active tone/voice
- Write in short paragraphs
- Use a large font (12-point minimum)
- Use bulleted lists instead of paragraphs when possible
When utilizing these verbal and written communication providers can help to make sure that patients fully understand what’s required of them, what things mean, and what questions to ask if they need clarification on anything.
Make Office Spaces More Patient-Friendly
It’s important to create a supportive environment for all patients. There are many ways that this can be accomplished, but a few suggestions are:
- Have a real person there to answer phones, collect information, and help patients schedule and prepare for their appointments
- Provide easy-to-read check-in forms, and help patients understand them and fill them out
- Provide directions to and for the referral and for any additional testing that a patient may need
- Provide all patient instructions and handouts in an easy-to-reach format
Following these four tips can help ease undo stress and anxiety that patients may experience while helping them to better understand exactly what’s going on.
What is the Provider’s Responsibility?
Providers who recognize that improving health literacy is, in part, their duty can make healthcare more approachable to patients while improving their outcomes.
Communication should be kept simple: following standard literacy guidelines and using technology that delivers easy-to-use resources in patient-friendly language will help patients understand their conditions and treatments better.
Offices should be organized with the patient in mind. It’s important that the patients feel taken care of from the moment they enter the office until the moment they leave. They should have the ability to ask someone questions at nearly anypoint in their visits, and should leave with a healthy understanding of their medical care and needs.
Following these steps to better communicate with patients ensures they understand their care.

David Thompson, MD, FACEP has more than two decades of experience working in the areas of clinical informatics, telehealth, decision support, NLP, and medical coding and documentation. A part-time faculty attending in the Northwestern Memorial Hospital Emergency Department, Dr. Thompson continues to enjoy both patient care and teaching. In a collaboration with well-known pediatrician Dr. Barton Schmitt (Schmitt-Thompson Clinical Content LLC), Dr. Thompson developed a comprehensive set of telephone triage guidelines that are used in medical call centers and doctors’ offices in the United States and internationally. Dr. Thompson was the Founder and CEO of Health Navigator. He has a BS in engineering and is board-certified in both internal medicine and emergency medicine, having completed a dual residency at Northwestern Memorial Hospital at Northwestern University. Dr. Thompson is a Fellow in the American College of Emergency Physicians.